Pethidine
 | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | oral, IV, IM |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 50-60% |
| Protein binding | 65-75% |
| Metabolism | Liver |
| Elimination half-life | 3-5 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.299 |
| Chemical and physical data | |
| Formula | C15H21NO2 |
| Molar mass | 247.33 g·mol−1 |
| 3D model (JSmol) | |
| |
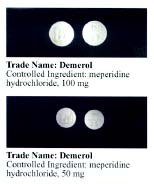
Pethidine (INN) or meperidine (USAN) (commonly referred to as Demerol but also referred to as: isonipecaine; lidol; pethanol; piridosal; Algil; Alodan; Centralgin; Dispadol; Dolantin; Petidin Dolargan (in Poland);[1] Dolestine; Dolosal; Dolsin; Mefedina) is a fast-acting opioid analgesic drug. In the United States and Canada, it is more commonly known as meperidine or by its brand name Demerol.[2]
Pethidine is indicated for the treatment of moderate to severe pain, and is delivered as its hydrochloride salt in tablets, as a syrup, or by intramuscular or intravenous injection. For much of the 20th century, pethidine was the opioid of choice for many physicians; in 1983 60% of doctors prescribed it for acute pain and 22% for chronic severe pain.[3] Compared to morphine, pethidine was supposed to be safer and carry less risk of addiction, and to be superior in treating the pain associated with biliary spasm or renal colic due to its putative antispasmodic effects. In fact, pethidine is no more effective than morphine at treating biliary or renal pain, and its low potency, short duration of action, and unique toxicity (i.e., seizures, delirium, other neuropsychological effects) relative to other available opioid analgesics have seen it fall out of favor in recent years for all but a very few, very specific indications.[4] Several countries, including Australia, have put severe limits on its use or curtailed it outright.[5] Nevertheless, some physicians continue to use it as a first-line strong opioid.
Pharmacodynamics/Mechanism of Action
Pethidine's efficacy as an analgesic was discovered almost accidentally; it was synthesized in 1939 as an antimuscarinic agent.[6] Pethidine also has structural similarities to atropine and other tropane alkaloids and may have some of their effects and side effects.[2] Pethidine exerts its analgesic effects by the same mechanism as morphine, by acting as an agonist at the μ-opioid receptor. In addition to its strong opioidergic and anticholinergic effects, it has local anesthetic activity related to its interactions with sodium ion channels. Pethidine's apparent in vitro efficacy as an "antispasmodic" is due to its local anesthetic effects. It does not, contrary to popular belief, have antispasmodic effects in vivo.[7] Pethidine also has stimulant effects mediated by its inhibition of the dopamine transporter (DAT) and norepinephrine transporter (NAT). Because of its DAT inhibitory action, pethidine will substitute for cocaine in animals trained to discriminate cocaine from saline.[8] Several analogues of pethidine have been synthesized that are potent inhibitors of the reuptake of the monoamine neurotransmitters dopamine and norepinephrine via DAT and NAT.[9][10] It has also been associated with cases of serotonin syndrome, suggesting some interaction with serotonergic neurons, but the relationship has not been definitively demonstrated.[5][6][8][10] It is more lipid-soluble than morphine, resulting in a faster onset of action. Its duration of clinical effect is 120-150 minutes. Despite producing analgesia for 2-3 hours at most, pethidine is typically administered at 4-6 hour intervals, so that the patient spends at least an hour (and up to four hours) between doses without any analgesia, resulting in much unnecessary pain and suffering. In addition, pethidine has been shown to be less effective than morphine, diamorphine or hydromorphone at easing severe pain, or pain associated with movement or coughing.[6][8][10] Like other opioid drugs, pethidine has the potential to cause physical dependence or addiction. In fact, pethidine may be more addictive than other opioids because of its exceptionally rapid onset of action and associated "rush", and additional activity as a monoamine transporter inhibitor, which results in cocaine-like stimulant effects in addition to its typical opioid effects.[11] When compared with oxycodone, hydromorphone, and placebo, pethidine was consistently associated with more euphoria, difficulty concentrating, confusion, and impaired psychomotor and cognitive performance when administered to healthy volunteers.[12] The especially severe side effects unique to pethidine among opioids — serotonin syndrome, seizures, delirium, dysphoria, tremor — are primarily or entirely due to the action of its metabolite, norpethidine.[6][10]
Pharmacokinetics
Pethidine is quickly hydrolysed in the liver to pethidinic acid and is also demethylated to norpethidine, which has half the analgesic activity of pethidine but a longer elimination half-life (8-12 hours[13]); accumulating with regular administration, or in renal failure. Norpethidine is toxic and has convulsant and hallucinogenic effects. The toxic effects mediated by the metabolites cannot be countered with opioid receptor antagonists such as naloxone or naltrexone and are probably primarily due to norpethidine's anticholinergic activity probably due to its structural similarity to atropine though its pharmacology has not been thoroughly explored. The neurotoxicity of pethidine's metabolites is a unique feature of pethidine compared to other opioids. Pethidine's metabolites are further conjugated with glucuronic acid and excreted into the urine.
Interactions
Pethidine has serious interactions that can be dangerous with MAOIs (e.g., furazolidone, isocarboxazid, moclobemide, phenelzine, procarbazine, selegiline, tranylcypromine). Such patients may suffer agitation, delirium, headache, convulsions, and/or hyperthermia. Fatal interactions have been reported including the death of Libby Zion.[14] It is thought to be caused by an increase in cerebral serotonin concentrations. It is possible that Pethidine can also interact with a number of other medications, including muscle relaxants, some antidepressants, benzodiazepines, and alcohol.
Pethidine is also relatively contraindicated for use when a patient is suffering from liver, or kidney disease, has a history of seizures or epilepsy, has an enlarged prostate or urinary retention problems, or suffers from hyperthyroidism, asthma, or Addison's disease.
Adverse effects
In addition to the adverse effects common to all opioids, such as constipation, dry mouth, lightheadedness, twitchiness, muscular twitches, and nausea, the repeated administration of pethidine can lead to neurotoxic effects. Pethidine should ideally not be administered by the intravenous route as there is a serious risk of triggering histamine release[citation needed].
References
- ^ "Lekopedia - Dolargan". jestemchory.pl. Retrieved 2006-08-01.
- ^ Demerol RxList. Retrieved 19 Jun. 2006.
- ^ Kaiko, Robert F. (1983). "Central Nervous System Excitatory Effects of Meperidine in Cancer Patients". Annals of Neurology. 13 (2). Wiley Interscience: 180–185. doi:10.1002/ana.410130213. ISSN: 0364-5134.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Donna Wong (2002-03-15). "Notes on Meperidine". Wong on Web Papers. Elsevier. Retrieved 2007-04-13.
{{cite web}}: CS1 maint: year (link) - ^ a b Davis, Sharon (2004). "Use of pethidine for pain management in the emergency department: a position statement of the NSW Therapeutic Advisory Group" (PDF). New South Wales Therapeutic Advisory Group. Retrieved 2007-01-17.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ a b c d Latta, Kenneth S. (January/February 2002). "Meperidine: A Critical Review". American Journal of Therapeutics. 9 (1). Lippincott Williams & Wilkins: 53–68. doi:10.1097/00045391-200201000-00010. ISSN: 1075-2765.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wagner, Larry E., II (1999). "Meperidine and Lidocaine Block of Recombinant Voltage-Dependent Na+ Channels: Evidence that Meperidine is a Local Anesthetic". Anesthesiology. 91 (5). Lippincott Williams & Wilkins: 1481–1490. doi:10.1097/00000542-199911000-00042. ISSN: 0003-3022.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Izenwasser, Sari (January/February 1996). "The cocaine-like behavioral effects of meperidine are mediated by activity at the dopamine transporter". European Journal of Pharmacology. 297 (1–2). Elsevier: 9–17. doi:10.1016/0014-2999(95)00696-6. ISSN: 0014-2999.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Lomenzo, Stacey A. (2005-03-05). "Synthesis and Biological Evaluation of Meperdine Analogs at Monoamine Transporters". Journal of Medicinal Chemistry. 48 (5). American Chemical Society: 1336–1343. doi:10.1021/jm0401614. ISSN: 0022-2623.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d "Demerol: Is It the Best Analgesic?" (PDF). Pennsylvania Patient Safety Reporting Service Patient Safety Advisory. 3 (2). Pennsylvania Patient Safety Authority. 2006. Retrieved 2007-01-16.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "In Brief". NPS Radar. National Prescribing Service. 2005. Retrieved 2007-01-17.
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help); Unknown parameter|month=ignored (help) - ^ Walker, Diana J. (1999). "Subjective, Psychomotor, and Physiological Effects of Cumulative Doses of Opioid µ Agonists in Healthy Volunteers". The Journal of Pharmacology and Experimental Therapeutics. 289 (3). American Society for Pharmacology and Experimental Therapeutics: 1454–1464.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Norpethedine half-life. 2002. Australian prescriber[1]
- ^ Brody, Jane (February 27, 2007). "A Mix of Medicines That Can Be Lethal". New York Times. Retrieved 2009-02-13.
The death of Libby Zion, an 18-year-old college student, in a New York hospital on March 5, 1984, led to a highly publicized court battle and created a cause célèbre over the lack of supervision of inexperienced and overworked young doctors. But only much later did experts zero in on the preventable disorder that apparently led to Ms. Zion's death: a form of drug poisoning called serotonin syndrome.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help)

