Cluster headache: Difference between revisions
| Line 137: | Line 137: | ||
Previously, vaso-constrictors such as [[ergot]] compounds were also used, and sufferers report a similar relief by taking strong cups of coffee immediately at the onset of an attack. |
Previously, vaso-constrictors such as [[ergot]] compounds were also used, and sufferers report a similar relief by taking strong cups of coffee immediately at the onset of an attack. |
||
Other abortive remedies that work for some include ice, hot showers, cool or lukewarm water sprayed on the face around the sinus, temple, and ear areas, breathing cold air, caffeine, and drinking large amounts of water in the early stages of an attack. Vigorous exercise has been shown in some cases to be very effective in relieving and aborting an acute attack by increasing the levels of oxygen within the body. This could also be due to an increase in adrenaline and changes in blood pressure. Some people report that sexual intercourse and specifically orgasm may terminate an attack possibly by acutely modulating hypothalamic function. Concentrating one's thoughts to a remote part of one's anatomy, such as the opposite little toe, reduced the length of attacks. Headaches are self-perpetuating by concentrating the mind on the symptoms.<!-- |
Other abortive remedies that work for some include ice, hot showers, cool or lukewarm water sprayed on the face around the sinus, temple, and ear areas, breathing cold air, application of White Flower analgesic balm beneath the nostrils, caffeine, and drinking large amounts of water in the early stages of an attack. Vigorous exercise has been shown in some cases to be very effective in relieving and aborting an acute attack by increasing the levels of oxygen within the body. This could also be due to an increase in adrenaline and changes in blood pressure. Some people report that sexual intercourse and specifically orgasm may terminate an attack possibly by acutely modulating hypothalamic function. Concentrating one's thoughts to a remote part of one's anatomy, such as the opposite little toe, reduced the length of attacks. Headaches are self-perpetuating by concentrating the mind on the symptoms.<!-- |
||
--><ref>{{cite journal |author=Ekbom K, Lindahl J |title=Effect of induced rise of blood pressure on pain in cluster headache |journal=Acta Neurol Scand |volume=46 |issue=4 |pages=585–600 |year=1970 |pmid=4994083 |doi=10.1111/j.1600-0404.1970.tb05815.x}}</ref><!-- |
--><ref>{{cite journal |author=Ekbom K, Lindahl J |title=Effect of induced rise of blood pressure on pain in cluster headache |journal=Acta Neurol Scand |volume=46 |issue=4 |pages=585–600 |year=1970 |pmid=4994083 |doi=10.1111/j.1600-0404.1970.tb05815.x}}</ref><!-- |
||
--><ref>{{cite journal |author=Atkinson R |title=Physical fitness and headache |journal=Headache |volume=17 |issue=5 |pages=189–91 |year=1977 |month=November |pmid=924787 |doi=10.1111/j.1526-4610.1977.hed1705189.x}}</ref><!-- |
--><ref>{{cite journal |author=Atkinson R |title=Physical fitness and headache |journal=Headache |volume=17 |issue=5 |pages=189–91 |year=1977 |month=November |pmid=924787 |doi=10.1111/j.1526-4610.1977.hed1705189.x}}</ref><!-- |
||
| Line 147: | Line 147: | ||
--><ref>{{cite journal |author=Nilsson Remahl AI, Ansjön R, Lind F, Waldenlind E |title=Hyperbaric oxygen treatment of active cluster headache: a double-blind placebo-controlled cross-over study |journal=Cephalalgia |volume=22 |issue=9 |pages=730–9 |year=2002 |month=November |pmid=12421159 |doi= 10.1046/j.1468-2982.2002.00450.x|url=http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0333-1024&date=2002&volume=22&issue=9&spage=730 |accessdate=2008-08-22}}</ref><!-- |
--><ref>{{cite journal |author=Nilsson Remahl AI, Ansjön R, Lind F, Waldenlind E |title=Hyperbaric oxygen treatment of active cluster headache: a double-blind placebo-controlled cross-over study |journal=Cephalalgia |volume=22 |issue=9 |pages=730–9 |year=2002 |month=November |pmid=12421159 |doi= 10.1046/j.1468-2982.2002.00450.x|url=http://www.blackwell-synergy.com/openurl?genre=article&sid=nlm:pubmed&issn=0333-1024&date=2002&volume=22&issue=9&spage=730 |accessdate=2008-08-22}}</ref><!-- |
||
--><ref>{{cite journal |author=Di Sabato F, Rocco M, Martelletti P, Giacovazzo M |title=Hyperbaric oxygen in chronic cluster headaches: influence on serotonergic pathways |journal=Undersea Hyperb Med |volume=24 |issue=2 |pages=117–22 |year=1997 |month=June |pmid=9171470 |doi= |url=http://archive.rubicon-foundation.org/2253 |accessdate=2008-08-22}}</ref> |
--><ref>{{cite journal |author=Di Sabato F, Rocco M, Martelletti P, Giacovazzo M |title=Hyperbaric oxygen in chronic cluster headaches: influence on serotonergic pathways |journal=Undersea Hyperb Med |volume=24 |issue=2 |pages=117–22 |year=1997 |month=June |pmid=9171470 |doi= |url=http://archive.rubicon-foundation.org/2253 |accessdate=2008-08-22}}</ref> |
||
===Prophylactic treatment=== |
===Prophylactic treatment=== |
||
Revision as of 17:39, 31 August 2009
| Cluster headache | |
|---|---|
| Specialty | Neurology |
| Frequency | 0.1% |
This headache disorder article lacks information pertaining to its ICHD-2 diagnostic criteria and/or classification. |
Cluster headache, nicknamed "suicide headache", is a neurological disease that involves, as its most prominent feature, an immense degree of pain. "Cluster" refers to the tendency of these headaches to occur periodically, with active periods interrupted by spontaneous remissions. The cause of the disease is currently unknown. It affects approximately 0.1% of the population, and men are more commonly affected than women.
Signs and symptoms
Cluster headaches are excruciating unilateral headaches,[1] of extreme intensity.[2] The duration of the common attack ranges from as short as 15 minutes to three hours or more. The onset of an attack is rapid, and most often without the preliminary signs that are characteristic of a migraine. However, some sufferers report preliminary sensations of pain in the general area of attack, often referred to as "shadows", that may warn them an attack is imminent. Though the headaches are almost exclusively unilateral, there are many documented as cases of "side-shifting" between cluster periods, or, even rarer, simultaneously (within the same cluster period) bilateral headache. They are often initially mistaken for brain tumors and multiple sclerosis until patients are treated with corticosteroids and then imaged. Trigeminal neuralgia can also bring on headaches with similar qualities. However, with Trigeminal neuralgia the pain is mostly located around the "cheek" area and is described as being more lance-like in quality.
Pain
The pain of cluster headaches is markedly greater than in other headache conditions, including severe migraines, and experts believe that it may be the most severe pain known to medical science. It has been described by female patients as being more severe than childbirth.[3] Dr. Peter Goadsby, Professor of Clinical Neurology at University College London, a leading researcher on the condition has commented, “Cluster headache is probably the worst pain that humans experience. I know that’s quite a strong remark to make, but if you ask a cluster headache patient if they’ve had a worse experience, they’ll universally say they haven’t. Women with cluster headache will tell you that an attack is worse than giving birth. So you can imagine that these people give birth without anesthetic once or twice a day, for six, eight or ten weeks at a time, and then have a break. It’s just awful.” [2] The pain is lancinating or boring in quality, and is located behind the eye (periorbital) or in the temple, sometimes radiating to the neck or shoulder. Analogies frequently used to describe the pain are a red-hot poker inserted into the eye, or a spike penetrating from the top of the head, behind one eye, radiating down to the neck, or sometimes having a leg amputated without any anaesthetic. The condition was originally named Horton's Neuralgia after Dr. B.T Horton, who postulated the first theory as to their pathogenesis. His original paper describes the severity of the headaches as being able to take normal men and force them to commit suicide. Indeed, cluster headaches are also known by the nickname "suicide headaches".
From Horton's 1939 original paper on cluster headache:
Our patients were disabled by the disorder and suffered from bouts of pain from two to twenty times a week. They had found no relief from the usual methods of treatment. Their pain was so severe that several of them had to be constantly watched for fear of suicide. Most of them were willing to submit to any operation which might bring relief.
Other symptoms
The cardinal symptoms of the cluster headache attack are ptosis (drooping eyelid), conjunctival injection (redness of the conjunctiva - the covering of the eyeball), lacrimation (tearing), rhinorrhea (runny nose), and, less commonly, facial blushing, swelling, or sweating. These features are known as the autonomic symptoms. The attack is also associated with restlessness, the sufferer often pacing the room or rocking back and forth. Less frequently, he or she will have an aversion to bright lights and loud noise during the attack. Nausea rarely accompanies a cluster headache, though it has been reported. The neck is often stiff or tender in the aftermath of a headache, with jaw or tooth pain sometimes present. Some sufferers report feeling as though their nose is stopped up and that they are unable to breathe out of one of their nostrils.
Cyclical recurrence and regular timing
Cluster headaches are occasionally referred to as "alarm clock headaches", because of its ability to wake a person from sleep, and because of the regularity of its timing in that both the individual attacks and the clusters themselves can have a metronomic regularity; attacks striking at a precise time of day each morning or night is typical, even precisely at the same time a week later. This has prompted researchers to speculate an involvement of the brain's "biological clock" or circadian rhythm.
Episodic or chronic
In episodic cluster headache, these attacks occur once or more daily, often at the same times each day, for a period of several weeks, followed by a headache-free period lasting weeks, months, or years. Approximately 10–15% of cluster headache sufferers are chronic; they can experience multiple headaches every day for years.
Cluster headaches occurring in two or more cluster periods lasting from 7 to 365 days with a pain-free remission of one month or longer between the clusters are considered episodic. If the attacks occur for more than a year without a pain-free remission of at least one month, the condition is considered chronic.[4] Chronic clusters run continuously without any "remission" periods between cycles. The condition may change from chronic to episodic and from episodic to chronic. Remission periods lasting for decades before the resumption of clusters have been known to occur.
Other names
The first complete description of cluster headache was given by the London neurologist Wilfred Harris in 1926. He named the disease Migrainous neuralgia.[5][6][7]
Cluster headaches have been called by several other names in the past including Erythroprosopalgia of Bing, Ciliary neuralgia, Erythromelagia of the head, Horton's headache (named after Bayard T. Horton, an American neurologist), Histaminic cephalalgia, Petrosal neuralgia, sphenopalatine neuralgia, Vidian neuralgia, Sluder's neuralgia, and Hemicrania angioparalyticia.[8] Sluder's neuralgia (syndrome) and cluster pain can often be temporarily stopped with nasal lidocaine drops.[9][10]
-
Robert Bing (1878–1956)
-
Bayard T. Horton (1895–1980)
Prevalence
While migraines are diagnosed more often in women, cluster headaches are diagnosed more often in men. The male-to-female ratio in cluster headache ranges from 4:1 to 7:1. It primarily occurs between the ages of 20 to 50 years.[11] This gap between the sexes has narrowed over the past few decades, and it is not clear whether cluster headaches are becoming more frequent in women, or whether they are merely being better diagnosed. Limited epidemiological studies have suggested prevalence rates of between 56 and 326 people per 100,000.[12] Latitude plays a role in the occurrence of cluster headaches, which are more common as one moves away from the equator towards the poles[citation needed].
Pathophysiology
Cluster headaches have been classified as vascular headaches. The intense pain is caused by the dilation of blood vessels which creates pressure on the trigeminal nerve. While this process is the immediate cause of the pain, the etiology (underlying cause or causes) is not fully understood.
Hypothalamus
Among the most widely accepted theories is that cluster headaches are due to an abnormality in the hypothalamus; Dr Goadsby, an Australian specialist in the disease has developed this theory. This can explain why cluster headaches frequently strike around the same time each day, and during a particular season, since one of the functions the hypothalamus performs is regulation of the biological clock. Metabolic abnormalities have also been reported in patients.
The hypothalamus is responsive to light—daylength and photoperiod; olfactory stimuli, including pheromones; steroids, including sex steroids and corticosteroids; neurally transmitted information arising in particular from the heart, the stomach, and the reproductive system; autonomic inputs; blood-borne stimuli, including leptin, ghrelin, angiotensin, insulin, pituitary hormones, cytokines, blood plasma concentrations of glucose and osmolarity, etc.; and stress. These particular sensitivities may underlay the causes, triggers, and methods of treatment of cluster headache.
 |
 |
 |
| Functional Magnetic Resonance Imaging (fMRI) shows brain areas being activated during pain | ||
 |
 |
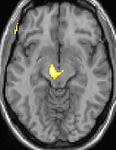 |
| Voxel-based morphometry (VBM) shows brain area structural differences | ||
The above fMRI pictures indicate the brain areas which are activated during pain only, compared to the pain free periods. These pictures show brain areas which are always active during pain in yellow/orange colour (called "pain matrix"). The area in the centre (in all three views) is specifically activated during cluster headache only. The bottom row Voxel-based morphometry (VBM) pictures show structural brain differences between cluster headache patients and people without headaches; only a portion of the hypothalamus is different.[13][14]
Genetics
There is a genetic component to cluster headaches, although no single gene has been identified as the cause. First-degree relatives of sufferers are more likely to have the condition than the population at large.[15] However, genetics appears to play a much smaller role in cluster headache than in some other types of headaches.
Triggers
Nitroglycerin (glyceryl trinitrate) can sometimes induce cluster headaches in sufferers in a manner similar to spontaneous attacks. Ingestion of alcohol or chocolate is recognized as a common trigger of cluster headaches when a person is in cycle or susceptible. Exposure to hydrocarbons (petroleum solvents, perfume) is also recognized as a trigger for cluster headaches. Some patients have a decreased tolerance to heat, and becoming overheated may act as a trigger which may explain the occurrence after aerobic exercise. Napping causes a headache for some sufferers, while for others lack of sleep triggers them. The role of diet and specific foods in triggering cluster headaches is controversial and not well understood.
Smoking
Nicotine may trigger cluster headaches, and the affliction is often found in people with a heavy addiction to cigarette smoking.[16]
Treatment
Cluster headaches often go undiagnosed for many years, being confused with migraine or other causes of headache.[17]
Medically, cluster headaches are considered benign, but because of the extreme and often debilitating pain associated with them, a severe attack is nevertheless treated as a medical emergency by doctors who are familiar with the condition. Because of the relative rareness of the condition and ambiguity of the symptoms, some sufferers may not receive treatment in the emergency room and patients may even be mistaken as exhibiting drug-seeking behavior.
Over-the-counter pain medications (such as aspirin, paracetamol, and ibuprofen) typically have no effect on the pain from a cluster headache. Unlike other headaches such as migraines and tension headaches, cluster headaches do not respond to biofeedback.
Medications to treat cluster headaches are classified as either abortives or prophylactics (preventatives). In addition, short-term transitional medications (such as steroids) may be used while prophylactic treatment is instituted and adjusted. With abortive treatments often only decreasing the duration of the headache and preventing it from reaching its peak rather than eliminating it entirely, preventive treatment is always indicated for cluster headaches, to be started at the first sign of a new cluster cycle.
Abortive treatment
During the onset of a cluster headache, some patients respond to rapid inhalation of pure oxygen (12-15 litres per minute in a non-rebreathing mask).[18] When used at the onset this can abort the attack in as little as 1 minute or as long as 10 minutes. Once an attack is at its peak, oxygen therapy appears to have little effect so most people have an oxygen provider close. Alternative first-line treatment is subcutaneous administration of triptan drugs, like sumatriptan and zolmitriptan.[18] The injectable form of sumatriptan has been shown to abort a cluster headache within fifteen minutes in 96% of cases.[19] Because of the rapid onset of an attack, the triptan drugs are usually taken by subcutaneous injection rather than by mouth. Newer medications in the triptan family such as Imitrix and Max-Alt are oral, non-injectables, and have a proven rate of successfully alleviating the peak pains in 15–20 minutes. Max-Alt is also available as a dissolvable tablet to be placed under the tongue. While its method claims to be fast acting due to this rapid absorption method, many sufferers are susceptible to the bitter and lingering aftertaste, further worsening the pain until the medication can take effect. While these oral medications are effective, they are also expensive. One prescription of 9 pills may run as high as $260. In some cases, doctors have tried the use of beta blockers as a treatment.
Some non-narcotic treatments that have shown mixed levels of success are botox injections along the occipital nerve, as well as sarapin (pitcher plant extract) injections.[20][21] Kudzu root (which has been demonstrated effective in some forms of migraine) has also been reported beneficial by many with cluster headaches. [22]
Recently, researchers have linked low testosterone as a possible cause of cluster headaches, which can be especially troublesome since the most effective pain medications for clusters, like morphine, reduce testosterone levels.[23][24]
Lidocaine and other topical anesthetics sprayed into the nasal cavity may relieve or stop the pain,[25] normally in a few minutes, but long term use is not suggested due to the side effects and possible damage to the nasal cavities.
Previously, vaso-constrictors such as ergot compounds were also used, and sufferers report a similar relief by taking strong cups of coffee immediately at the onset of an attack.
Other abortive remedies that work for some include ice, hot showers, cool or lukewarm water sprayed on the face around the sinus, temple, and ear areas, breathing cold air, application of White Flower analgesic balm beneath the nostrils, caffeine, and drinking large amounts of water in the early stages of an attack. Vigorous exercise has been shown in some cases to be very effective in relieving and aborting an acute attack by increasing the levels of oxygen within the body. This could also be due to an increase in adrenaline and changes in blood pressure. Some people report that sexual intercourse and specifically orgasm may terminate an attack possibly by acutely modulating hypothalamic function. Concentrating one's thoughts to a remote part of one's anatomy, such as the opposite little toe, reduced the length of attacks. Headaches are self-perpetuating by concentrating the mind on the symptoms.[26][27][28]
Hyperbaric oxygen therapy has been used successfully in treating cluster headaches though it was not shown to be more successful than surface oxygen.[29][30][31]
Prophylactic treatment
A wide variety of prophylactic medicines are in use, and patient response to these is highly variable. Current European guidelines suggest the use of the calcium channel blocker verapamil at a dose of at least 240 mg daily. Steroids, such as prednisolone, are also effective, with a high dose given for the first five days or longer before tapering down. Methysergide, lithium and the anticonvulsant topiramate are recommended as alternative treatments.[18]
Muscle relaxants and atypical anti-psychotics have also been used.
Magnesium supplements have been shown to be of some benefit in about 40% of patients.[32] Melatonin has also been demonstrated to bring significant improvement in approximately half of episodic patients. [33]
Other neuropathic pain alleviating agents can also be used such as the Tricyclic antidepressants including Amitriptyline and Nortriptyline
Non-established and research approaches
There is substantial anecdotal evidence that serotonergic psychedelics such as psilocybin (mushrooms) and LSD and LSA (d-Lysergic acid amide, contained by Rivea corymbosa seeds) abort cluster periods and extend remission periods.[34][35][36] Melatonin, psilocybin, serotonin, and the triptan abortive drugs are closely-related tryptamines.
Dr. Andrew Sewell and Dr. John Halpern at McLean Hospital in Boston have investigated the ability of psilocybin ("magic mushrooms") and LSD to treat cluster headaches. These researchers examined medical records of 53 patients who had taken hallucinogenic mushrooms and reported in Neurology that the majority of them found partial or complete relief from cluster attacks.[37] A clinical study of these treatments under the auspices of Clusterbusters is being developed by Dr. Halpern and colleagues at Harvard Medical School, McLean Hospital.[38][39]
Within the United States, the Controlled Substances Act (CSA) of 1970 makes it illegal to possess hallucinogens (including psilocybin and LSD), classifying them as Schedule I drugs with no legitimate medical use. Patients who use psilocybin to treat their symptoms face legal prosecution, although there are no known convictions.
Other types of headache
- Chronic Paroxysmal Hemicrania (CPH) is a condition similar to cluster headache, but CPH responds well to treatment with the anti-inflammatory drug indomethacin and the attacks are much shorter, often lasting only seconds.[40]
- Some people with extreme headaches of this nature (especially if they are not unilateral) may actually have an ictal headache. Anti-convulsant medications can significantly improve this condition so sufferers should consult a physician about this possibility.[41]
- It is also possible to have two or more different types of headaches, complicating diagnosis and treatment.
See also
- Tension headaches
- Migraine
- Rebound headaches
- Hemicrania continua
- Trigeminal neuralgia
- Chronic Paroxysmal Hemicrania
- Organization for Understanding Cluster Headaches
- Clusterheadaches.com, worldwide cluster headache support group
- Clusterbusters.com, cluster headache research and education foundation
References
- ^ Beck E, Sieber WJ, Trejo R (2005). "Management of cluster headache". Am Fam Physician. 71 (4): 717–24. PMID 15742909.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Capobianco DJ, Dodick DW (2006). "Diagnosis and treatment of cluster headache". Semin Neurol. 26 (2): 242–59. doi:10.1055/s-2006-939925. PMID 16628535.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Matharu M, Goadsby P (2001). "Cluster Headache -- Update on a Common Neurological Problem" (PDF). Practical Neurology. 1: 42–9. doi:10.1046/j.1474-7766.2001.00505.x.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ IHS Classification ICHD-II 3.1.2 Chronic cluster headache
- ^ Harris W.: Neuritis and Neuralgia. Oxford: Oxford Univ.Press; 1926
- ^ Bickerstaff ER (1959). "The periodic migrainous neuralgia of Wilfred Harris". Lancet. 1 (7082): 1069–71. doi:10.1016/S0140-6736(59)90651-8. PMID 13655672.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Boes CJ, Capobianco DJ, Matharu MS, Goadsby PJ (2002). "Wilfred Harris' early description of cluster headache". Cephalalgia. 22 (4): 320–6. doi:10.1046/j.1468-2982.2002.00360.x. PMID 12100097.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Stephen D. Silberstein, Richard B. Lipton. Peter J. Goadsgy. "Headache in Clinical Practice." Second edition. Taylor & Francis. 2002.
- ^ Kittrelle JP, Grouse DS, Seybold ME (1985). "Cluster headache. Local anesthetic abortive agents". Arch. Neurol. 42 (5): 496–8. PMID 3994568.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Costa A, Pucci E, Antonaci F; et al. (2000). "The effect of intranasal cocaine and lidocaine on nitroglycerin-induced attacks in cluster headache". Cephalalgia. 20 (2): 85–91. doi:10.1046/j.1468-2982.2000.00026.x. PMID 10961763.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ [1]
- ^ Torelli P, Castellini P, Cucurachi L, Devetak M, Lambru G, Manzoni G (2006). "Cluster headache prevalence: methodological considerations. A review of the literature". Acta Biomed Ateneo Parmense. 77 (1): 4–9. PMID 16856701.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ May A, Bahra A, Büchel C, Frackowiak RS, Goadsby PJ (2000). "PET and MRA findings in cluster headache and MRA in experimental pain". Neurology. 55 (9): 1328–35. PMID 11087776.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ DaSilva AF, Goadsby PJ, Borsook D (2007). "Cluster headache: a review of neuroimaging findings". Curr Pain Headache Rep. 11 (2): 131–6. doi:10.1007/s11916-007-0010-1. PMID 17367592.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pinessi L, Rainero I, Rivoiro C, Rubino E, Gallone S (2005). "Genetics of cluster headache: an update". J Headache Pain. 6 (4): 234–6. doi:10.1007/s10194-005-0194-x. PMID 16362673.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Schürks M, Diener HC (2008). "Cluster headache and lifestyle habits". Curr Pain Headache Rep. 12 (2): 115–21. doi:10.1007/s11916-008-0022-5. PMID 18474191.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Vast Majority of Cluster Headache Patients Are Initially Misdiagnosed, Dutch Researchers Report". World Headache Alliance. 2003-08-21. Retrieved 2006-10-08.
- ^ a b c May A, Leone M, Afra J, Linde M, Sándor P, Evers S, Goadsby P (2006). "EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias". Eur J Neurol. 13 (10): 1066–77. doi:10.1111/j.1468-1331.2006.01566.x. PMID 16987158.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) Free Full Text (PDF) - ^ Treatment of acute cluster headache with sumatriptan. The Sumatriptan Cluster Headache Study Group. N Engl J Med 1991;325:322-6.
- ^ Sostak P, Krause P, Förderreuther S, Reinisch V, Straube A (2007). "Botulinum toxin type-A therapy in cluster headache: an open study". J Headache Pain. 8 (4): 236–41. doi:10.1007/s10194-007-0400-0. PMID 17901920.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Interview with Dr. Jeff Baird: Treating Migraines with Medical Acupuncture". American Academy of Medical Acupuncture. Retrieved 2008-08-24.
- ^ Sewell RA.: Response of Cluster Headache to Kudzu. Headache. Published Online: 9 Oct 2008; DOI.
- ^ Stillman MJ (2006). "Testosterone replacement therapy for treatment refractory cluster headache". Headache. 46 (6): 925–33. doi:10.1111/j.1526-4610.2006.00436.x. PMID 16732838. Retrieved 2008-08-24.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ceccarelli I, De Padova AM, Fiorenzani P, Massafra C, Aloisi AM (2006). "Single opioid administration modifies gonadal steroids in both the CNS and plasma of male rats". Neuroscience. 140 (3): 929–37. doi:10.1016/j.neuroscience.2006.02.044. PMID 16580783. Retrieved 2008-08-24.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mills T, Scoggin J (1997). "Intranasal lidocaine for migraine and cluster headaches". Ann Pharmacother. 31 (7–8): 914–5. PMID 9220056.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ekbom K, Lindahl J (1970). "Effect of induced rise of blood pressure on pain in cluster headache". Acta Neurol Scand. 46 (4): 585–600. doi:10.1111/j.1600-0404.1970.tb05815.x. PMID 4994083.
- ^ Atkinson R (1977). "Physical fitness and headache". Headache. 17 (5): 189–91. doi:10.1111/j.1526-4610.1977.hed1705189.x. PMID 924787.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Gotkine M, Steiner I, Biran I. (2006). "Now dear, I have a headache! Immediate improvement of cluster headaches after sexual activity". J Neurol Neurosurg Psychiatry. 77 (11): 1296. doi:10.1136/jnnp.2006.092643. PMID 17043304.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)- Abstract - ^ Bennett MH, French C, Schnabel A, Wasiak J, Kranke P (2008). "Normobaric and hyperbaric oxygen therapy for migraine and cluster headache". Cochrane Database Syst Rev (3): CD005219. doi:10.1002/14651858.CD005219.pub2. PMID 18646121.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Nilsson Remahl AI, Ansjön R, Lind F, Waldenlind E (2002). "Hyperbaric oxygen treatment of active cluster headache: a double-blind placebo-controlled cross-over study". Cephalalgia. 22 (9): 730–9. doi:10.1046/j.1468-2982.2002.00450.x. PMID 12421159. Retrieved 2008-08-22.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Di Sabato F, Rocco M, Martelletti P, Giacovazzo M (1997). "Hyperbaric oxygen in chronic cluster headaches: influence on serotonergic pathways". Undersea Hyperb Med. 24 (2): 117–22. PMID 9171470. Retrieved 2008-08-22.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Mauskop A, Altura BT, Cracco RQ, Altura BM (1995). "Intravenous magnesium sulfate relieves cluster headaches in patients with low serum ionized magnesium levels". Headache. 35 (10): 597–600. doi:10.1111/j.1526-4610.1995.hed3510597.x. PMID 8550360.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Leone M; et al. (19965). "Melatonin versus placebo in the prophylaxis of cluster headache: a double-blind pilot study with parallel groups". Cephalalgia. 16 (7): 494–496. doi:10.1046/j.1468-2982.1996.1607494.x. PMID 8933994.
{{cite journal}}:|access-date=requires|url=(help); Check date values in:|year=(help); Explicit use of et al. in:|author=(help)CS1 maint: year (link) - ^ "Hallucinogenic Treatment of Neuro-Vascular Headaches". ClusterBusters. Retrieved 2006-09-22.
- ^ Mark Honigsbaum (2005-08-02). "Headache sufferers flout new drug law - Calls for clinical trials and rethink of legislation as patients claim that magic mushrooms can relieve excruciating condition". The Guardian. Retrieved 2006-09-22. [reprint by Multidisciplinary Association for Psychedelic Studies]
- ^ Arran Frood (2008-10-07). "LSD cured my headache - Cluster headaches cause such severe pain that some sufferers are driven to suicide. Now one man believes he's found a surprising cure". The Independent. Retrieved 2008-10-07.
- ^ Sewell R, Halpern J, Pope H (2006). "Response of cluster headache to psilocybin and LSD". Neurology. 66 (12): 1920–2. doi:10.1212/01.wnl.0000219761.05466.43. PMID 16801660.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - a Brief Communications, also presented as:
Sewell, R. Andrew, M.D.; Halpern, John M., M.D. "The Effects Of Psilocybin And LSD On Cluster Headache: A Series Of 53 Cases." Abstract. Presented to the National Headache Foundation’s Annual Headache Research Summit. February, 2006. - ^ "Research into psilocybin and LSD as potential treatments for people with cluster headaches". LSD and Psilocybin Research. Multidisciplinary Association for Psychedelic Studies. Retrieved 2006-09-22.
- ^ "Response of Cluster Headache to Psilocybin and LSD" Chapter 5 in "Psychedelic Medicine: New Evidence for Hallucinogens as Treatment" Michael Winkelman and Thomas B. Roberts (editors) (2007) Westport, CT: Praeger/Greenwood.
- ^ NEURO/67 at eMedicine
- ^ "Seizures and Headaches: They Don't Have to Go Together". Epilepsy.com. 2003-09-16. Retrieved 2006-09-22.
This website is not associated with any medical or scientific organization and has nothing to do with any research pertaining to cluster headache syndrome.
External links
- Clusterheadaches.com, worldwide cluster headache support group
- Algorithm for diagnosis and treatment from National Guideline Clearinghouse (DHHS)
- The International Headache Society (IHS): 2nd Edition of The International Headache Classification (ICHD-2) - 3.1 Cluster Headache
- Organisation for the Understanding of Cluster Headache (UK)
- Association Française Contre l'Algie Vasculaire de la Face (FR)



